Typhoid Fever Outbreak 2025: Key Symptoms, Latest Diagnostic Tools & What You Need to Know About Salmonella Typhi
Introduction
Typhoid diagnosis refers to the process of identifying the presence of Salmonella Typhi, the bacterium responsible for causing typhoid fever. Accurate diagnosis is crucial for timely treatment and preventing complications. The diagnosis of typhoid fever typically begins with a detailed assessment of symptoms such as high fever, abdominal pain, fatigue, and constipation or diarrhea. Laboratory confirmation is essential, with common tests including the Widal test, which detects antibodies, and TyphiDot, a rapid diagnostic tool that identifies specific IgM and IgG antibodies against Salmonella Typhi. Blood cultures remain the gold standard, especially in the early stages of the disease, while stool and urine cultures may also help in later stages. Advanced molecular methods like PCR (Polymerase Chain Reaction) are increasingly being used for faster and more precise results. Early and accurate diagnosis of typhoid fever ensures prompt antibiotic treatment, reduces transmission, and improves patient outcomes, especially in areas with frequent outbreaks or poor sanitation.
Understanding Typhoid Fever: A Global Health Concern
Salmonella enterica serotype Typhi is a Gram-negative bacterium transmitted via the fecal-oral route, often through contaminated food or water. While typhoid fever has long been a concern in parts of South Asia and Africa, 2025 has seen a concerning global uptick, including in urban regions with previously stable public health systems. A combination of antibiotic resistance, climate-driven changes in sanitation infrastructure, and population movement has contributed to the outbreak. Even more worrying are the evolving clinical presentations, complicating timely diagnosis and treatment.
The Cause: Salmonella Typhi
Salmonella Typhi is a gram-negative, motile bacillus that invades the intestinal mucosa and spreads systemically through the bloodstream. Once it breaches the gut-associated lymphoid tissue, it can reach various organs like the liver, spleen, and bone marrow. Unlike other strains of Salmonella that cause gastroenteritis, S. Typhi exclusively infects humans and can persist in asymptomatic carriers, making its control more complex.
Key Symptoms of Typhoid Fever in 2025
Recognizing the early warning signs of typhoid fever is crucial in limiting complications and initiating timely treatment. The clinical presentation of typhoid can vary in severity but typically includes:
-
Persistent high-grade fever (often rising in a step-ladder pattern)
-
Severe abdominal pain and cramping
-
Headache and weakness
-
Constipation or diarrhea (more commonly diarrhea in children)
-
Rose-colored spots on the abdomen and chest
-
Enlarged spleen and liver (hepatosplenomegaly)
-
Loss of appetite and weight loss
-
Mental dullness, confusion, or delirium in advanced stages
Emerging Strains and Antimicrobial Resistance
The 2025 outbreak has brought to light a surge in Multi-Drug Resistant (MDR) and Extensively Drug-Resistant (XDR) Salmonella Typhi strains, particularly in Pakistan, India, and several African nations. These strains exhibit resistance to first-line antibiotics such as ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole, and even newer fluoroquinolones and third-generation cephalosporins.
This resistance necessitates the use of costlier and more toxic antibiotics like carbapenems and azithromycin, posing serious challenges in resource-limited settings.
Latest Diagnostic Tools for Typhoid Fever in 2025
Accurate and early diagnosis remains pivotal in managing and containing typhoid fever. In 2025, advancements in diagnostic tools have significantly improved detection rates, reducing the chances of misdiagnosis.
1. Blood Culture
-
Still considered the gold standard for typhoid diagnosis.
-
Most reliable within the first week of illness.
-
Sensitivity: ~60%
-
Limitations: Requires lab infrastructure and takes 2–3 days.
2. Typhoid Rapid Diagnostic Tests (RDTs)
-
Examples: TUBEX TF, TyphiDot, and Test-it Typhoid IgM
-
Detect IgM/IgG antibodies against S. Typhi antigens.
-
Provide results within 15–30 minutes.
-
Suitable for field settings and rural areas.
-
Improved specificity and sensitivity over older Widal tests.
3. Polymerase Chain Reaction (PCR)
-
Detects S. Typhi DNA directly from blood or stool samples.
-
High sensitivity and specificity (over 90%)
-
Used in central diagnostic labs due to cost and equipment needs.
-
Especially useful for detecting MDR and XDR strains.
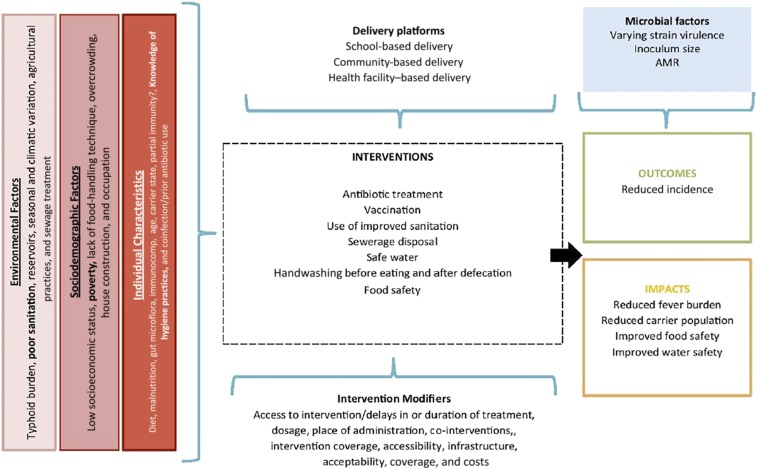
How Typhoid Spreads: Transmission Pathways
Typhoid fever spreads via the fecal-oral route, meaning that any contaminated water, food, or surface can become a vehicle for the bacteria. Common routes include:
-
Drinking untreated or improperly stored water
-
Eating raw vegetables or fruits washed in contaminated water
-
Handling food by infected individuals without proper hand hygiene
-
Contact with asymptomatic carriers who shed the bacteria in stool
Prevention Strategies: Breaking the Transmission Cycle
To mitigate the spread of typhoid in 2025, coordinated public health interventions and individual preventive measures are necessary:
1. Vaccination
-
Typhoid Conjugate Vaccines (TCVs) like Typbar-TCV are recommended by WHO for children above 6 months.
-
Single-dose vaccines provide protection for up to 5 years.
-
Mass immunization programs in high-risk areas have shown significant success.
2. Safe Drinking Water and Sanitation
-
Boiling water or using certified water purification systems.
-
Avoiding street food and uncooked meals.
-
Promoting handwashing with soap after using the toilet and before meals.
3. Surveillance and Carrier Identification
-
Regular screening of food handlers and healthcare workers.
-
Treatment of chronic carriers with appropriate antibiotics.
-
Public health surveillance to map hotspots and contain outbreaks.
Treatment Guidelines for Typhoid Fever in 2025
Due to the increasing prevalence of drug resistance, antibiotic stewardship is essential. Treatment should be guided by antibiotic susceptibility testing (AST).
Recommended First-line Treatments (based on AST results):
-
Azithromycin: For uncomplicated MDR typhoid.
-
Ceftriaxone or cefotaxime: For hospitalized patients or XDR cases.
-
Meropenem: Reserved for severe XDR typhoid with systemic complications.
-
Supportive therapy: Includes hydration, electrolyte correction, and fever control.
Complications of Untreated or Severe Typhoid
If not diagnosed and treated promptly, typhoid can lead to life-threatening complications, including:
-
Intestinal perforation and peritonitis
-
Sepsis and septic shock
-
Meningitis or encephalopathy
-
Myocarditis and endocarditis
-
Bone infections (osteomyelitis) in chronic cases
-
Relapse and chronic carriage
Typhoid in Children: Special Considerations
Children under five are particularly vulnerable to complications, with atypical symptoms like:
-
High fever with prolonged lethargy
-
Sudden vomiting or diarrhea
-
Dehydration and rapid weight loss
-
Convulsions or unconsciousness in severe cases
Pediatric vaccination, regular nutrition monitoring, and parental awareness campaigns remain critical.
Global Response: WHO & Local Authorities
The World Health Organization (WHO), in collaboration with CDC, UNICEF, and national health ministries, is:
-
Promoting universal access to TCVs
-
Supporting countries with rapid diagnostics and outbreak response kits
-
Funding sanitation infrastructure projects in high-risk zones
-
Deploying epidemiologists and mobile clinics to outbreak regions
What You Need to Do Now
Given the rising tide of typhoid fever cases in 2025, individuals and institutions must:
-
Ensure clean drinking water supply
-
Implement strict hygiene protocols
-
Get vaccinated, especially before traveling to endemic regions
-
Advocate for public health funding in sanitation and diagnostics
-
Educate communities through school, workplace, and media campaigns